What is hypoxic-ischemic encephalopathy (HIE)?
Hypoxic-ischemic encephalopathy (HIE) is a type of newborn brain damage caused by oxygen deprivation and limited blood flow. HIE is a type of birth injury; this is a broad term used to refer to any harm that a baby experiences at or near the time of birth. Other terms used for HIE include birth asphyxia, perinatal asphyxia, and neonatal encephalopathy.
In some cases, therapeutic hypothermia can prevent or minimize permanent brain damage, although it must be given within just hours of the baby’s birth/oxygen-depriving injury (see our page on “Treatment for HIE” for more information). However, with and without therapeutic hypothermia, many infants with HIE can go on to develop permanent health conditions and disorders, such as cerebral palsy (CP), cognitive disabilities, epilepsy, hearing and vision impairments.
What can HIE mean for my baby’s future?
The full extent of a child’s injuries from HIE are typically not apparent immediately after birth, for two major reasons:
-
- Brain injury from HIE is an evolving process. When blood flow is cut off to parts of the brain, cells begin to break down, die, and release substances which are toxic to other cells. These cells then begin to die off and continue the chain reaction, which causes brain injury to spread over a period of hours or days. Therapeutic hypothermia can help to disrupt this chain reaction.
- Damage from HIE may occasionally not become apparent until a child has developmental delays. For example, impacts on mobility may not be noticed until the child struggles to meet milestones such as crawling or walking.
Once there is permanent brain damage, there is no cure for HIE . However, there are many treatments and therapies that can improve symptoms and function in children with HIE.
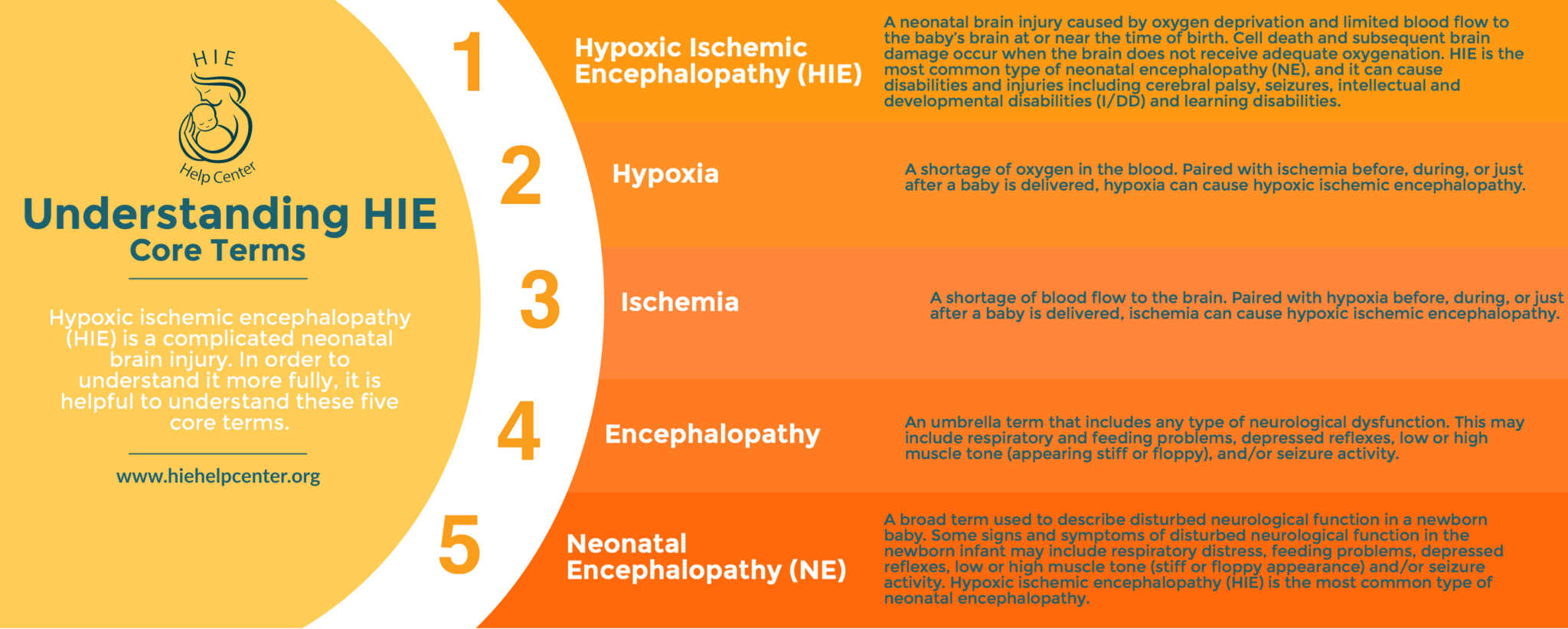
Terminology Related to HIE
What are the causes of HIE?
HIE can be caused by a variety of medical complications around the time of birth. In many cases, medical malpractice also plays a role. For example, doctors may fail to properly monitor the health of the mother and baby and identify potential issues. Alternatively, they may recognize problems but not take them seriously enough/fail to intervene. Learn more information on the association between HIE and malpractice, as well as legal options.
The following health problems and negligent actions can lead to HIE (these are just a few examples; for more information please see this page):

- Mismanagement of a high-risk pregnancy: Women with conditions such as preeclampsia and gestational diabetes require more extensive monitoring and treatment.
- Umbilical cord complications: The umbilical cord is like a lifeline between mother and baby, supplying oxygen and nutrients and removing fetal waste. Anything that compresses the cord or reduces its function puts the baby at risk of HIE.
- Placental or uterine complications: The placenta and uterus also play very important roles in providing oxygenated blood to the baby. Examples of placental and uterine issues that may cause HIE include:
- Placental abruption: when the placenta separates from the uterus before the baby is born
- Placenta previa: when the placenta attaches too close to the cervix; this can cause dangerous bleeding and oxygen deprivation during delivery
- Placental insufficiency: when the placenta is unable to deliver enough blood to the baby
- Uterine rupture: when the uterus tears, partially or completely
- Infections: Infections in the mother can spread to the baby during labor and delivery, especially if the medical team do not take adequate precautions (such as doing indicated infection screening and prescribing antibiotics when needed).
- Improper fetal heart monitoring: If a baby shows signs of fetal distress on the fetal heart monitor, doctors and nurses can often intervene so that their oxygen supply is restored. If necessary, this may involve an emergency C-section. However, if monitoring is sporadic or does not occur, important signs of danger may be missed.
- Failure to prevent a premature birth: Premature babies are at higher risk for HIE and other birth injuries because their lungs are so underdeveloped. Therefore, it is very important that doctors do what they can to prevent premature birth, such as performing a cervical cerclage (a stitch placed in the cervix to stop it from opening too early) or providing progesterone treatment.
- Allowing prolonged labor to continue: Labor is stressful for babies because uterine contractions compress the placenta and umbilical cord that supply their oxygen. If something is preventing labor from progressing, and physicians do not offer intervention (such as an emergency C-section), this is negligence. Prolonged labor is more likely to occur when a baby is larger than normal, or the mother’s pelvis is smaller than normal.
- Medication problems: Sometimes physicians prescribe medications such as Pitocin and Cytotec in order to induce or enhance labor. Unfortunately, these medications can also cause uterine contractions to become so strong and frequent that the baby is dangerously deprived of oxygen.
- Mismanagement of a neonatal condition: Hypoxic-ischemic injury can be caused by complications during the neonatal period, i.e. a baby’s first month of life. Problems such as respiratory distress, jaundice, and neonatal hypoglycemia can all contribute to an HIE diagnosis, especially if mismanaged.
What are the signs and symptoms of HIE?
Babies with HIE may exhibit any of the following signs (among others):
- Breathing problems
- Feeding problems
- Missing reflexes (for example, the baby does not respond to loud noises)
- Seizures
- Low Apgar scores
- Low or high muscle tone
- Altered level of consciousness (e.g. not alert)
How do you pronounce hypoxic-ischemic encephalopathy (HIE)?
Treatment for HIE
HIE is managed using a treatment called therapeutic hypothermia, where the baby’s brain or body is cooled down below normal temperatures to slow the cascade effect that causes widespread damage. This allows the baby’s brain to recover and reduces the level of disability they may have as they grow. According to current guidelines, the treatment must be given within six hours of birth, although there is some evidence to suggest it may be beneficial when given up to 24 hours.
This allows the baby’s brain to recover and reduces the level of disability they may have as they grow. According to current guidelines, the treatment must be given within six hours of birth, although there is some evidence to suggest it may be beneficial when given up to 24 hours.
Therapeutic hypothermia lasts for around 72 hours, allowing the baby’s metabolic rate to slow. This prevents further damage known as reperfusion injury, which occurs when normal oxygenation and blood flow are restored too quickly to the brain’s cells. While it may seem counter-intuitive that restoring flow quickly could cause further injury, the brain’s cells react differently to rapid oxygenation after being oxygen deprived. After oxygen deprivation injury, rapid oxygenation can cause more inflammation and the release of certain harmful compounds. Hypothermia treatment works to stabilize the brain’s cells and prevent or limit damaging inflammation.
In addition to therapeutic hypothermia, medical staff should provide supportive care, which can mean helping the baby breathe, controlling and preventing seizures and low blood sugar, minimizing brain swelling, and more. In the long term, babies with brain damage from HIE may benefit from a wide variety of treatments and therapies. Although these are not curative, they can minimize symptoms and maximize function. Click here for more information.
Types and forms of HIE

If they suspect HIE, medical staff can conduct brain imaging, such as ultrasound and MRI, to see how badly tissue in the brain is damaged. Caregivers also do a blood gas test to determine the pH of the baby’s blood, which can also provide some information about the baby’s oxygen levels.
The severity of HIE is determined using Sarnat staging, which takes into account clinical presentation, exam results, seizure presence, and illness duration. Mild HIE is classified as Sarnat Grade I, and severity increases up to a maximal Stage III (1).
Prevalence and incidence of HIE
HIE is estimated to occur in between 2 to 9 per 1,000 live births. The advent of therapeutic hypothermia has significantly reduced rates of death and disability, but outcomes can still be severe. In one study, nearly half of newborns with HIE either died or had a major neurodevelopmental disability at an 18-month follow-up. However, 40 percent of babies in this study had normal early development (2).
Life expectancy for people with HIE and cerebral palsy
The life expectancy of people with hypoxic-ischemic encephalopathy depends greatly on the extent to which they are affected and their access to treatments and therapies. For this reason, it’s difficult provide an “average” lifespan for people with HIE. Because many children with HIE are also diagnosed with cerebral palsy, it may be more useful to look at life expectancies for people with cerebral palsy.
People with very mild cerebral palsy are typically expected to live as long as their peers in the general population. Overall, life expectancy for a person with cerebral palsy depends on the extent to which they are affected:
- Lifespan of mild cerebral palsy: For people with fairly mild cerebral palsy (defined as walking unaided), life expectancy in females has been estimated at 70-80 years, and in males at 66-76 years.
- Lifespan of severe cerebral palsy: For those who are more severely affected (defined as an inability to lift the head and being fed through a tube), life expectancies have been estimated to be shorter for both females and males, depending on the quality of medical care received.
These lifespan numbers were extracted from a 2008 study in Developmental Medicine and Child Neurology. Click here to view the paper, which contains a detailed table on life expectancy for people with cerebral palsy. It takes into account age, sex, movement ability, and feeding mechanism (3).
More detailed information on HIE
For more information on HIE, please visit our Medical Information section.
About the HIE Help Center and ABC Law Centers
The HIE Help Center is run by ABC Law Centers, a medical malpractice firm exclusively handling cases involving HIE and other birth injuries. Our lawyers have over 100 years of combined experience with this type of law, and have been advocating for children with HIE and related disabilities since the firm’s inception in 1997.
We are passionate about helping families obtain the compensation necessary to cover their extensive medical bills, loss of wages (if one or both parents have to miss work in order to care for their child), assistive technology, and other necessities.
If you suspect your child’s HIE may have been caused by medical negligence, please contact us today to learn more about pursuing a case. We provide free legal consultations, during which we will inform you of your legal options and answer any questions you have. Moreover, you would pay nothing throughout the entire legal process unless we obtain a favorable settlement.
You are also welcome to reach out to us with inquiries that are not related to malpractice. We cannot provide individualized medical advice, but we’re happy to track down informational resources for you.
Citations
- Sarnat, H. B., & Sarnat, M. S. (1976). Neonatal encephalopathy following fetal distress: a clinical and electroencephalographic study. Archives of neurology, 33(10), 696-705.
- (n.d.). Retrieved January 15, 2019, from https://www.uptodate.com/contents/clinical-features-diagnosis-and-treatment-of-neonatal-encephalopathy
- Strauss, D., Brooks, J., Rosenbloom, L., & Shavelle, R. (2008). Life expectancy in cerebral palsy: an update. Developmental Medicine & Child Neurology, 50(7), 487-493.