Hypoxic-ischemic encephalopathy (HIE) is caused by brain injury from not getting enough oxygen to the brain. A hypoxic-ischemic injury most commonly occurs at or around the time of birth.
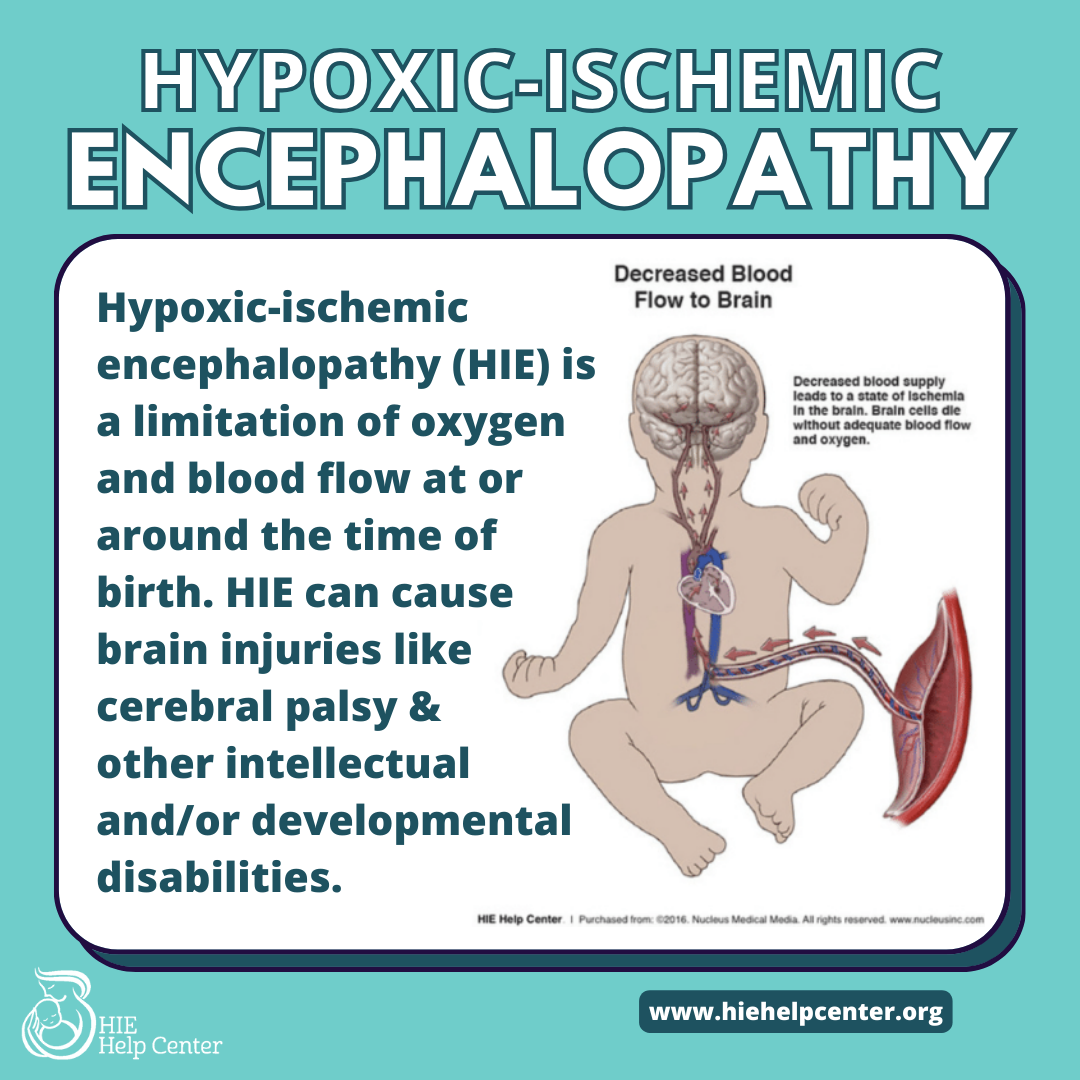
Occasionally, HIE may not be preventable. However, in most cases, HIE is preventable and is caused by oxygen deprivation and HIE due to medical negligence. In those situations, medical staff misses or mismanages a pregnancy, birth, or delivery issue and does not deliver in time. A variety of conditions can cause HIE, including the following.
Jump to:
- High-Risk Pregnancy and HIE
- HIE from Umbilical Cord Issues
- HIE From Placental or Uterine Complications
- HIE from Cervical Issues
- HIE from Oligohydramnios and Polyhydramnios
- HIE from Infections in the Mother or Baby
- HIE from Intrauterine Growth Restriction (IUGR)
- HIE from Labor and Delivery Errors
- HIE from Neonatal Health Mismanagement
High-Risk Pregnancy and HIE

“High-risk pregnancy” encompasses a variety of conditions that require close monitoring and possible intervention. With proper medical management, women with high-risk pregnancies often deliver healthy babies. However, the health of the mother and baby may be in danger if medical professionals don’t recognize high risk pregnancies and risk factors and manage these situations appropriately. These conditions require extra attention and care.
Complications that cause HIE can arise if doctors do not closely monitor a high risk pregnancy. In such cases, a baby can suffer HIE from not getting enough oxygen. These situations could otherwise be prevented with extra care and check-ups. Physicians should also many times consult with high risk specialists to make sure the pregnancy goes smoothly and the baby arrives healthy.
HIE from Umbilical Cord Issues
- The umbilical cord is the baby’s sole source of oxygen and nutrients. It is considered the baby’s lifeline while in the mom’s uterus. If the umbilical cord is torn, blocked, compressed, or knotted, the baby may not get enough oxygen.Examples of umbilical cord issues include:
- Nuchal cord: When the umbilical cord is wrapped around the baby’s neck.
- Umbilical cord prolapse: When the umbilical cord exits the uterus before the baby does.
- Short cord: When the umbilical cord is abnormally short, it may restrict the baby’s movement and development. A short umbilical cord can also cause the placenta to become detached from the uterus (placental abruption).
- True knot: a knot that forms in an umbilical cord.
- Infected or inflamed cord: If the umbilical cord becomes infected, it can cause serious problems for the baby, including HIE.
Vasa previa: This is a condition where blood vessels move into the membranes that lie across the birth canal. During labor and delivery, these vessels may rupture. The resulting blood loss can cause HIE.
HIE from Placental or Uterine Complications
The umbilical cord is attached to the placenta. The placenta transports nutrients and oxygen from the uterus to the baby through the umbilical cord. Issues with the uterus, placenta, or umbilical cord can limit the flow of oxygen and nutrients, which will put the baby at risk for HIE.
Uterine and placental complications that may cause HIE include:
HIE from Uterine Rupture
In rare cases, a mother’s uterus may tear (rupture) during delivery, which is accompanied by massive bleeding. Uterine rupture can happen when a mother attempts a vaginal birth with uterine scarring from a prior C-section, surgery, or other procedure.
During uterine rupture, the baby can lose oxygen due to:
- Massive bleeding and loss of blood flow to the baby
- The mother’s blood pressure dropping sharply
- Moving out of the uterus and into the abdominal cavity and stretching, compressing, or tearing the umbilical cord
Uterine rupture is associated with placental abruption. Both conditions require delivery via emergency C-section.
HIE from Placental Abruption
Usually, the placenta stays attached to the uterus until delivery. In a placental abruption, the placenta separates from the uterus early. If this happens, oxygen and blood flow to the baby will be decreased. The baby may not get enough oxygen, causing HIE. The severity of an abruption can vary, but a mild abruption can turn severe very quickly.
HIE from Placenta Previa
In most cases, the placenta connects to the uterus far away from the mother’s cervix. With placenta previa, however, the placenta attaches to the uterus close to the cervix.
Placenta previa can cause life-threatening bleeding during delivery. Physicians can detect this condition if a mother reports on-and-off bleeding during the second half of her pregnancy. Ultrasound can confirm the diagnosis.
In some cases, a low-lying placenta moves out of the way as the pregnancy progresses. If it does not, delivering early, via C-section can reduce the risk of HIE. With placenta previa, the baby may also suffer from blood loss and require an emergency blood transfusion.
HIE from Placental Insufficiency
Placental insufficiency is when the placenta can’t deliver enough blood to the baby. This may be due to issues such as gestational diabetes, hypertension and preeclampsia and the baby is at risk for intrauterine growth restriction (IUGR) and the mother may have oligohydramnios (low amniotic fluid). Placental insufficiency may result in oxygen deprivation and HIE if a baby is not delivered in time.
Doctors should be monitoring these pregnancies closely with several tests, measurements, and ultrasounds, including:
- non-stress tests
- biophysical profiles
- ultrasounds to measure the baby’s size
- ultrasounds to measure amniotic fluid levels
- Ultrasounds to gauge placental structure
- Doppler ultrasounds to see how blood is flowing to the baby
HIE from Cervical Issues
The cervix is a structure between the uterus and vagina that normally stays closed during pregnancy. If it’s too short or the tissue is weakened, it may be a condition called cervical insufficiency.The cervix can open too early, causing premature rupture of membranes and an extremely premature birth with a high risk of HIE.
In many cases, there are no symptoms, but doctors are responsible for screening for risk factors, such as:
- prior cervical insufficiency
- a history of D&C (dilation and curettage) procedures
- previous traumatic birth
- prior premature rupture of membranes
- uterine anomalies
If a mother has risk factors, doctors should perform a physical exam and multiple transvaginal ultrasound studies (TVS) over time to track cervix length. Doctors can also use cervical cerclage or progesterone treatment to help prevent preterm labor and delivery.
HIE from Oligohydramnios and Polyhydramnios
Oligohydramnios is a complication characterized by too little amniotic fluid.
Polyhydramnios is when there is too much amniotic fluid.
If there is too little or too much amniotic fluid, the umbilical cord function may become compromised, increasing the risk of HIE. Doctors should be screening for amniotic fluid issues with physical examinations and ultrasound during the pregnancy.
HIE from Infections in the Mother or Baby
Infections may cause abnormalities in fetal heart monitoring and can cause seizures, HIE, and even require the baby to be admitted to the NICU (Neonatal Intensive Care Unit) if a baby is not delivered in time. In many cases, adequate screening, proper preventative measures, and timely delivery can prevent injury from not getting enough oxygen or infection.
If a mother has an active infection during delivery, doctors should give antibiotics or acyclovir. It may also be necessary to deliver via C-section before the membranes rupture, so the baby is not exposed to infection via vaginal delivery. Some of these infections include:
- Chorioamnionitis and villitis
- Group B strep
- Bacterial vaginosis
- Herpes simplex virus (HSV, also known as genital herpes)
Depending on what the infection is, the baby may be diagnosed differently. Diagnoses related to infection include:
- Sepsis: an infection that circulates through the blood and tissues
- meningitis: inflammation of the membranes around the brain and spinal cord
- encephalitis: brain inflammation caused by a virus
- pneumonia: bacterial lung infection that can cause the baby to develop breathing issues and oxygen deprivation
HIE from Intrauterine Growth Restriction (IUGR)
If a baby isn’t growing enough during pregnancy, there may be IUGR. Medical staff should screen for this problem with regularly-scheduled ultrasounds and other tests such as Doppler flow, weight checks, amniocentesis, non-stress tests, and biophysical profiles.
Once diagnosed, IUGR babies must be closely monitored and delivered early, as many of them do not do well in labor. Lack of close monitoring and timely delivery can result in HIE.
HIE from Labor and Delivery Errors
During labor, complications require prompt responses from medical teams for emergency intervention. Failure to follow proper protocols can result in HIE.
Common labor and delivery errors include:
Improperly monitoring a baby’s heart rate
It’s standard practice to start fetal monitoring once a mother is admitted to the labor and delivery ward. Fetal monitoring helps doctors and nurses watch the baby’s heart rate and tell whether a baby is getting enough oxygen. If the baby’s heart rate drops or is non-reassuring, it may mean the baby is having fetal distress, and not getting enough oxygen which can lead to HIE.
Monitoring requires staff to be able to recognize and properly read heart tracings to tell whether a baby is getting enough oxygen. If medical personnel fails to recognize signs of distress or respond in time, it is possible a baby will suffer HIE.
Failing to prevent a preterm birth
Premature birth is a known risk factor for HIE. Premature babies are not done developing yet, and their brains are more fragile and susceptible to injury. There are interventions that doctors should perform to help prevent premature birth.
Failing to properly manage premature rupture of membranes (PROM)
PROM occurs if a mother’s membranes rupture (‘water breaks’) more than 18 hours before labor starts. This can pose a risk for HIE and other birth injuries because the amniotic fluid that protects the baby from infection is gone. Doctors should:
- administer antibiotics to decrease the risk of infection
- Potentially deliver via C-section
- administer corticosteroids to mature the baby’s lungs if they are preterm.
Screening for infections can help prevent PROM and premature PROM, when the membranes rupture before 37 weeks of gestation.
Prolonging a pregnancy for too long
If a baby is not born after 40 weeks, this may be considered a post-term pregnancy. After around 37 weeks, the placenta starts to break down in preparation for delivery. If a baby is in the womb for too long, it can be exposed to low-oxygen conditions as the placenta continues to deteriorate. The baby may develop postmaturity syndrome, which increases risk of complications.
Prolonging labor and delivery for too long
Every pregnancy and labor is different, but there are certain indicators that labor is progressing normally. If labor is stalled, some medical interventions might be necessary to help the mother deliver the baby safely.
Traumatic birth
Traumatic birth occurs when a baby is injured in the birthing process due to too much mechanical force. Common reasons for traumatic birth include:
- Attempting vaginal delivery when the baby:
- Is in a face position or breech position
- Is too big to fit through the mother’s pelvis
- Has a shoulder stuck on the mother’s pelvic bones
- Excessive uterine contractions stimulated by induction drugs like Pitocin or Cytotec
- Improper technique when using forceps or a vacuum extractor
If there are known complications with the baby’s size, position, or the labor is stalling, doctors should move onto a C-section. Waiting too long to deliver can cause HIE.
HIE from Neonatal Health Mismanagement
Babies can develop health issues after birth that require timely intervention. Incorrect or delayed treatment can make these health issues much worse. In many cases, however, these complications can be prevented with proper monitoring and adherence to standards of care. These health issues include:
Neonatal breathing problems
Babies who have gone through a difficult birth sometimes need help breathing. If resuscitation does not work, they are placed on a breathing machine called a ventilator. Medical staff must place the tube properly and regulate the pressure of gases going to the baby’s lungs.
If medical staff manage the ventilator treatment improperly, the baby can have devastating complications:
- A misplaced tube not delivering air to the baby’s lungs at all
- stomach tears
- lung collapse
- the lungs getting too distended and injured to work (pneumothorax)
Improper treatment of meconium aspiration syndrome (MAS)
MAS is an emergency. In MAS, the baby inhales particles of his or her stool during labor, which can:
- block airways
- decrease oxygen to the baby’s brain
- cause infection
- Cause pneumonia.
Babies with respiratory distress and MAS are admitted to the NICU, and are treated with some combination of:
- Airway clearance
- Ventilation
- Supplemental oxygen
- Surfactant therapy
- Steroid therapy
- Nitric oxide
- ECMO or radiant warmer to maintain their body temperature
The level and extent of treatment depends on the severity of the baby’s respiratory distress. If the baby’s MAS is not treated properly, they may suffer from HIE due to oxygen deprivation.
Improperly treating jaundice and kernicterus
Babies can develop yellow skin (jaundice), poor feeding, and lethargy after birth. Jaundice is caused by increased concentrations of bilirubin, a product of the breakdown of red blood cells. Babies may need help to safely remove this bilirubin, especially if it develops in the first 24 hours after birth or between days 3-7 of life.
Medical staff place the babies under special blue lights or under a fiber optic blanket in a process called phototherapy. This is a noninvasive and easy treatment which should prevent jaundice from getting worse. If the bilirubin level becomes too high, exchange transfusions will be needed.
If jaundice isn’t recognized in time or the proper treatment is not given, bilirubin can cross the blood-brain barrier and cause kernicterus, a form of brain damage, which often overlaps with HIE.
Improper treatment of neonatal hypoglycemia
A baby’s developing brain depends exclusively on glucose for energy. Low blood sugar levels can cause brain cells to die, leading to brain bleeds and HIE. This is one of the most common neonatal health issues, and one of the most easily solved with extra feedings (breastmilk or formula) or glucose solution via IV in extreme situations.
Hypoglycemia can occur due to:
- Too much insulin (a disorder called PHHI)
- Intrauterine growth restriction (when the baby is small for their gestational age)
- Premature birth
- Abnormally high body temperature (hyperthermia)
- Abnormally high red blood cell mass (polycythemia)
- Sepsis (bloodstream infection)
- Growth hormone deficiency
- Dysfunctions in the glucose generation or breakdown pathways
- Depleted glycogen levels (due to oxygen deprivation or starvation)
If a baby is at risk for hypoglycemia or shows signs of hypoglycemia, doctors should measure their blood glucose concentration within minutes and treat them promptly.
Do you need someone to talk to?
Your child was just diagnosed with HIE. Your head is spinning with what may feel like a thousand different things. Questions, medical terms, care plans–it can be difficult to make sense of everything that has happened.
We want to hear your story. HIE Help Center is owned by ABC Law Centers, a birth injury law firm. Our intake team is here to listen to every detail of what you and your family may have gone through during labor and delivery. Although we are not doctors and cannot provide medical advice, our team can provide you with resources specifically tailored to your situation. Our team has reviewed and handled thousands of cases and is trained to recognize if there may have been medical malpractice that lead to your child’s diagnosis, and we can advise if taking legal action may be beneficial to you and your family.
