Disclaimer: We cannot provide treatments or medical advice. Please call 911, your country’s emergency number, or your doctor if you may be having a medical emergency.
What is fetal distress?
 Fetal distress, also called “nonreassuring fetal status,” is the term medical professionals use to describe when a fetus is not receiving adequate oxygen during pregnancy or labor (1). Fetal distress is an indication that the baby may not be doing well in utero. When a baby is in distress they may require immediate intervention, such as delivery by C-section or certain methods of intrauterine resuscitation. If fetal distress goes unmanaged it can lead to more severe injuries such as hypoxic-ischemic encephalopathy (HIE).
Fetal distress, also called “nonreassuring fetal status,” is the term medical professionals use to describe when a fetus is not receiving adequate oxygen during pregnancy or labor (1). Fetal distress is an indication that the baby may not be doing well in utero. When a baby is in distress they may require immediate intervention, such as delivery by C-section or certain methods of intrauterine resuscitation. If fetal distress goes unmanaged it can lead to more severe injuries such as hypoxic-ischemic encephalopathy (HIE).
Terminology
According to an American College of Obstetricians and Gynecologists (ACOG) Committee Opinion in 2005, the term fetal distress was deemed too confusing, as it was very similar to “birth asphyxia” (2). However, many doctors still use the phrase. Birth asphyxia means that the baby is not receiving adequate oxygen during labor or delivery because of an issue like cord compression, placental abruption, or another birth complication. In fetal distress, the baby appears to be lacking adequate oxygen based on fetal heart rate, though the cause may not be known. Instead, the term “nonreassuring fetal status” has been more commonly used to describe the clinician or doctor’s interpretation of the data related to fetal status.
Causes of fetal distress
Some common causes of fetal distress can include (1):
- Anemia
- Intrauterine growth restriction (IUGR)
- Post-term pregnancy (pregnancy at 42 weeks or more)
- Meconium-stained amniotic fluid
- Oligohydramnios (low amniotic fluid)
- Pregnancy-induced hypertension
Signs of fetal distress
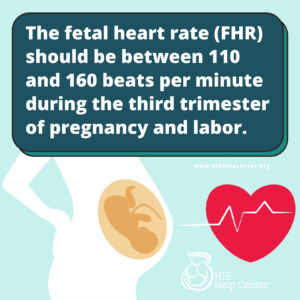
Fetal distress is diagnosed based on fetal heart rate monitoring. The fetal heart rate should be monitored throughout pregnancy and taken at every prenatal appointment. Doctors can use internal or external tools to measure the fetal heart rate (1). It is most commonly measured via electronic fetal monitor. The fetal heart rate should be between 110 and 160 beats per minute during the third trimester of pregnancy and labor.
Heart rate abnormalities that are signs of fetal distress:
- Tachycardia (an abnormally fast heart rate)
- Bradycardia (an abnormally slow heart rate)
- Variable decelerations (abrupt decreases in heart rate)
- Late decelerations (late returns to the baseline heart rate after a contraction)
All of these circumstances need to be monitored closely by your doctor (1).
 Life-long complications may be a result of medical negligence. Our legal team has over 20 years of experience getting justice for children with birth injuries resulting from fetal distress. You may have a case.
Life-long complications may be a result of medical negligence. Our legal team has over 20 years of experience getting justice for children with birth injuries resulting from fetal distress. You may have a case.
Other pregnancy concerns that can increase the risk of fetal distress
Fetal heart rate monitoring is the way that doctors diagnose fetal distress. Other common pregnancy concerns, however, can also signify that the fetus is in trouble. These include:
Decreased fetal movement
Fetal movement is an important sign that a baby is in good health (3,4). A baby’s movements usually become established around 28 weeks into the pregnancy; during this time there is both movement and stillness, as babies sleep and rest in the womb.
 During prenatal appointments, medical professionals should ask an expectant mother if her baby’s movements have stopped, slowed, or decreased, since changes in fetal movement can be a sign of fetal distress. If fetal movement is decreased the physician should perform prenatal tests such as non-stress tests (NST), biophysical profiles (BPP), and/or ultrasounds to observe the baby in the womb.
During prenatal appointments, medical professionals should ask an expectant mother if her baby’s movements have stopped, slowed, or decreased, since changes in fetal movement can be a sign of fetal distress. If fetal movement is decreased the physician should perform prenatal tests such as non-stress tests (NST), biophysical profiles (BPP), and/or ultrasounds to observe the baby in the womb.
Cramping
As a baby grows and the uterus expands, mothers will often experience cramping. Doctors should advise mothers to report cramping as soon as it occurs, especially if cramping is severe and if back pain is also present. Intense cramping may be an indication of a serious complication – such as placental abruption – that may cause fetal distress (5).
Vaginal bleeding
Certain conditions such as placenta previa, vasa previa, and placental abruption can cause bleeding during pregnancy (6). Depending on the severity of these issues, they may all cause fetal distress. Due to this, medical professionals should pay attention to maternal reports of vaginal bleeding as it may be an indication of a more serious condition that could lead to fetal distress.
Maternal weight gain
It is important for mothers and their physicians to pay attention to how much weight gain occurs during pregnancy. Experts state weight gain between 25 and 40 pounds during pregnancy is normal (7). Pregnancy weight gain outside of this range might lead to fetal distress.
Abnormal results of biophysical profile (BPP)
The BPP is measured via ultrasound. The ultrasound technician will collect four measurements: fetal breathing, amniotic fluid volume, fetal movement, and fetal tone (8). Each measurement is given a score of 0 or 2, and a composite score of less than 4 reveals fetal compromise.
Abnormal amniotic fluid levels
Amniotic fluid is one of the main indicators of fetal health (9). Amniotic fluid volume (AFV) can measure too low (oligohydramnios), or too high (polyhydramnios). These abnormalities can be signs of congenital abnormalities, uteroplacental insufficiency, fetal chromosomal abnormalities, cord compression, and others.
What to do in cases of fetal distress
Medical personnel must closely monitor all pregnancies, especially high-risk pregnancies, and continuously assess the health of the mother and baby. When physicians recognize or are alerted to signs of fetal distress, they can monitor the baby and decide how to proceed in the safest way. Usually the doctor will do this using fetal heart rate (FHR) monitoring. FHR allows the doctor to monitor signs of hypoxia, the response of the fetus to hypoxia, and the mother’s contractions (1).
Once a baby experiences signs of fetal distress on monitoring, the main goal is to return the baby to an oxygen-rich state as soon as possible to avoid the risk of injury. Sometimes, the best way to alleviate fetal distress is to deliver, thereby removing the baby from an oxygen-deprived environment. C-section delivery may be the safest way for this to occur.
Fetal distress and HIE
Fetal distress occurs when the baby is not well in the womb. Oftentimes fetal distress occurs when a baby is cut off from its oxygen supply, leading to oxygen deprivation. Medical professionals must address the signs of fetal distress immediately in order to prevent the occurrence of hypoxic-ischemic encephalopathy (HIE). If fetal distress is left unmanaged, and HIE occurs, it can lead to long-term, permanent brain injury for the baby. HIE is associated with an increased risk of other long-term health issues including:
- Cerebral palsy
- Epilepsy and seizure disorders
- Intellectual and developmental disabilities (I/DD)
- Behavioral and emotional disorders
- Hearing and visual impairments
Additional reading
About the HIE Help Center and ABC Law Centers
The HIE Help Center is run by ABC Law Centers, a medical malpractice firm exclusively handling cases involving HIE and other birth injuries. Our lawyers have over 100 years of combined experience with this type of law, and have been advocating for children with HIE and related disabilities since the firm’s inception in 1997.
We are passionate about helping families obtain the compensation necessary to cover their extensive medical bills, loss of wages (if one or both parents have to miss work in order to care for their child), assistive technology, and other necessities.
If you suspect your child’s HIE may have been caused by medical negligence, please contact us today to learn more about pursuing a case. We provide free legal consultations, during which we will inform you of your legal options and answer any questions you have. Moreover, you would pay nothing throughout the entire legal process unless we obtain a favorable settlement.
You are also welcome to reach out to us with inquiries that are not related to malpractice. We cannot provide individualized medical advice, but we’re happy to track down informational resources for you.
Sources
- Fetal Distress: Diagnosis, Conditions & Treatment. (2016, May 19). Retrieved March 27, 2024, from https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/fetal-distress/
- What are the Signs of Fetal Distress. (2014). Retrieved March 27, 2024, from https://www.abclawcenters.com/frequently-asked-questions/what-are-some-signs-that-my-baby-is-in-distress/
- Inappropriate use of the terms fetal distress and birth asphyxia. ACOG Committee Opinion No. 326. American College of Obstetricians and Gynecologists. Obstet Gynecol 2005;106:1469-70.
- WhattoExpect. (2022, October 27). Fetal Distress During Pregnancy & Labor. Retrieved March 27, 2024, from https://www.whattoexpect.com/pregnancy/pregnancy-health/complications/fetal-distress.aspx
- Hofmeyr, G. J., & Novikova, N. (2012). Management of reported decreased fetal movements for improving pregnancy outcomes. The Cochrane database of systematic reviews, 4, CD009148.
- Cramping During Pregnancy: Causes, Treatment & Prevention. (2017, February 22). Retrieved March 27, 2024, from https://americanpregnancy.org/your-pregnancy/cramping-during-pregnancy/
- Ananth, C. V., & Kinzler, W. L. (2022, July). Acute placental abruption: Pathophysiology, clinical features, diagnosis, and consequences. Retrieved March 27, 2024, from https://www.uptodate.com/contents/acute-placental-abruption-pathophysiology-clinical-features-diagnosis-and-consequences
- Reproductive Health. (2022, June 13). Retrieved from https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-weight-gain.htm
- Manning, F. A. (2023, May). Biophysical profile test for antepartum fetal assessment. Retrieved March 27, 2024, from https://www.uptodate.com/contents/biophysical-profile-test-for-antepartum-fetal-assessment
- Magann, E., & Ross, M. G. (2024, February). Assessment of amniotic fluid volume. Retrieved March 27, 2024, from https://www.uptodate.com/contents/assessment-of-amniotic-fluid-volume

Leave a Reply
You must be logged in to post a comment.