Hypothermia therapy is one established treatment that can minimize permanent brain damage from hypoxic-ischemic encephalopathy (HIE). However, it must be given very shortly after birth/the oxygen-depriving incident in order to be effective (ideally within six hours). This treatment is known as hypothermia therapy, but it has many other names, such as “therapeutic hypothermia,” “cooling therapy,” and “neonatal cooling.”
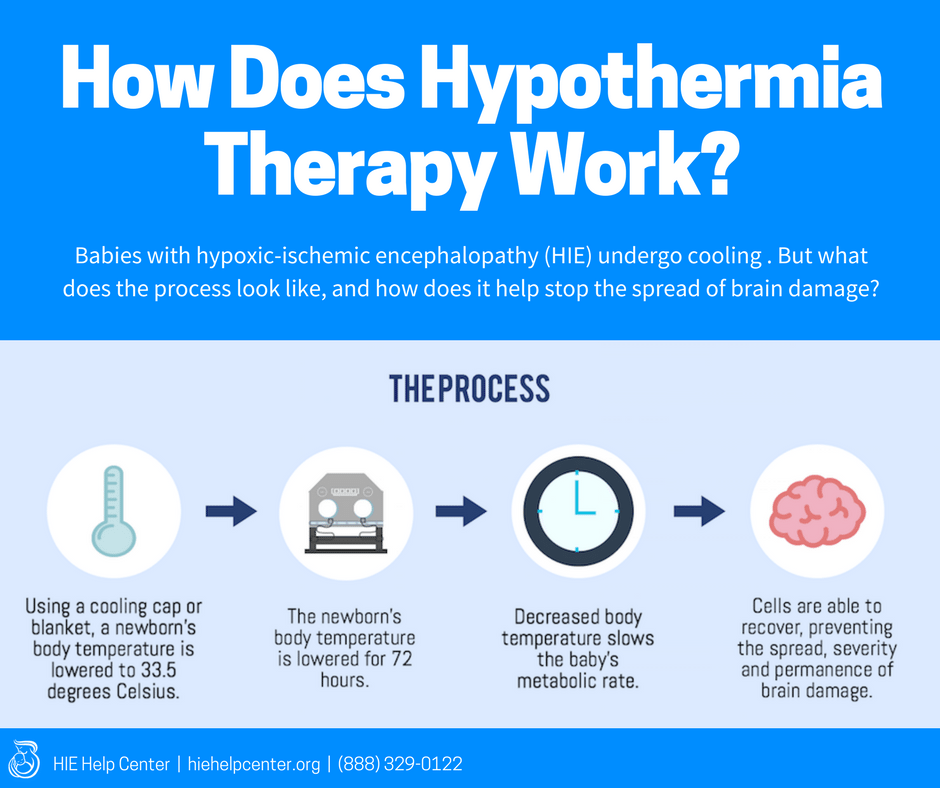
 Hypothermia therapy involves cooling the baby down to a temperature below homeostasis to allow the brain to recover from a hypoxic-ischemic injury. Typically, the target temperature is about 33.5 degrees Celsius (92.3 degrees Fahrenheit) (1).
Hypothermia therapy involves cooling the baby down to a temperature below homeostasis to allow the brain to recover from a hypoxic-ischemic injury. Typically, the target temperature is about 33.5 degrees Celsius (92.3 degrees Fahrenheit) (1).
There are two ways that hypothermia therapy can be administered:
- Using a cooling cap for “selective brain cooling” or
- By cooling the baby’s entire body (“whole-body cooling”)
Either of these options can be effective; the choice to use one over the other is dependent on what protocols are in place and what equipment a particular NICU has (2).
Jump To:
- Care during hypothermia therapy
- How does hypothermia therapy work?
- When should my baby get hypothermia therapy?
- Re-warming the baby after hypothermia therapy
- Where do babies get hypothermia therapy?
- About the HIE Help Center and ABC Law Centers
Care during hypothermia therapy
Before, during, and after hypothermia therapy, medical professionals must carefully monitor the baby’s health and provide interventions if necessary. Among other things, this may entail:
- Conducting blood gas tests and managing acidosis (excessive acid in the blood)
- Maintaining normal glucose and electrolyte levels
- Providing respiratory and cardiovascular support as needed
- Testing for and treating infections
- Maintaining sedation at an appropriate level
- EEG monitoring (for signs of seizure activity) and controlling seizures
How does hypothermia therapy work?
When should my baby get hypothermia therapy?
If your baby was diagnosed with hypoxic-ischemic encephalopathy (HIE), doctors have to begin hypothermia therapy very shortly after the oxygen deprivation occurred. Hypothermia therapy should ideally be commenced within six hours of birth, under certain circumstances, this may be done within 12 hours (2).
The sooner hypothermia therapy begins, the greater the chance that the baby’s potential disabilities will be minimized. There are certain criteria that babies have to meet in order to qualify for the therapy, and these can vary slightly depending on the hospital your baby is in. Babies that meet one or more the following criteria should be given therapeutic hypothermia (2):

- An oxygen-depriving complication/birth injury occurred
- The baby’s Apgar score (at 10 minutes of life) was five or lower
- The baby underwent prolonged resuscitation
- The baby experienced severe acidosis
- The baby had an abnormal umbilical or neonatal blood gas test result
Additionally, one or both of the following:
- The baby had seizures
- The baby was showing clinical signs of brain damage
Failure to provide hypothermia therapy to a baby that needs it is medical malpractice. It is important to note that, in many cases, HIE itself may be caused by malpractice.
Re-warming the baby after hypothermia therapy
Although the exact ways that hypothermia therapy protects the brain are not fully known, one of the purported benefits is that it reduces the chance of reperfusion injury. Reperfusion injury occurs when blood flow is restored too quickly to injured parts of the brain; this can worsen brain damage (3).
After therapeutic hypothermia, the baby must be rewarmed slowly in order to prevent reperfusion injury. The baby’s temperature should be increased by 0.2 – 0.5 degrees Celsius, until it reaches 36.5 degrees Celsius. Because there is an increased risk of seizure activity during rewarming, doctors should also consider EEG monitoring (2).
Where do babies get hypothermia therapy?
Not all hospitals will be equipped to provide therapeutic hypothermia because not all NICUs are the same. Community hospitals, for example, may not have brain cooling equipment, but they should have the ability to transfer the baby to a bigger or more specialized hospital that can provide cooling. It is a good idea to inquire about what kind of care a neonatal care unit can provide when researching hospitals.
*Research update: the window of time to provide hypothermia therapy may be longer than previously thought
Traditionally, it has been thought that hypothermia therapy must be administered within six hours of birth in order to be effective. However, recent research indicates that this may not be the case (4). Laptook et al. (2017) set out to investigate whether hypothermia therapy given six to 24 hours after birth could benefit infants with HIE. They conducted a randomized clinical trial on 168 infants with moderate or severe HIE. Their results were inconclusive. However, Bayesian analysis indicated that hypothermia therapy may have slightly reduced the chance of death and disability.
The authors call for further research on the window of time in which hypothermia therapy can be effective, stressing that if belated administration of hypothermia therapy is even slightly better than no hypothermia therapy, that knowledge would still be profoundly important. Of course, the neuroprotective effects of cooling treatment are stronger the sooner it is given, so medical professionals should still administer it as quickly as possible.
About the HIE Help Center
The HIE Help Center is run by ABC Law Centers (Reiter & Walsh, P.C.), a medical malpractice firm exclusively handling cases involving HIE and other birth injuries since the firm’s inception in 1997.
If you suspect your child’s HIE may have been caused by medical negligence, please contact us today to learn more about pursuing a case. We provide free legal consultations, during which we will inform you of your legal options and answer any questions you have. Moreover, you would pay nothing throughout the entire legal process unless we obtain a favorable settlement.
Related reading:
Sources
- Wu, Y. (n.d.). Clinical features, diagnosis, and treatment of neonatal encephalopathy. Retrieved May 14, 2024, from https://www.uptodate.com/contents/clinical-features-diagnosis-and-treatment-of-neonatal-encephalopathy
- The Academica Medical Center Patient Safety Organization (AMC PSO) Neonatal Encephalopathy Task Force. (2016). Therapeutic Hypothermia in Neonates: Recommendations of the Neonatal Encephalopathy Task Force[Pamphlet].
- Wintermark, P., Hansen, A., Gregas, M. C., Soul, J., Labrecque, M., Robertson, R. L., & Warfield, S. K. (2011). Brain perfusion in asphyxiated newborns treated with therapeutic hypothermia. American Journal of Neuroradiology, 32(11), 2023-2029.
- Laptook, A. R., Shankaran, S., Tyson, J. E., Munoz, B., Bell, E. F., Goldberg, R. N., … & Das, A. (2017). Effect of therapeutic hypothermia initiated after 6 hours of age on death or disability among newborns with hypoxic-ischemic encephalopathy: a randomized clinical trial. Jama, 318(16), 1550-1560.