Why is fetal heart monitoring important?
 When a mother is admitted into the labor and delivery unit, the hospital’s doctors and nurses must monitor the baby’s heart rate continuously. This is critical because fetal heart rate indicates how well a baby is handling labor and is the best way to tell whether the baby is getting enough oxygen.
When a mother is admitted into the labor and delivery unit, the hospital’s doctors and nurses must monitor the baby’s heart rate continuously. This is critical because fetal heart rate indicates how well a baby is handling labor and is the best way to tell whether the baby is getting enough oxygen.
Sometimes, there is insufficient flow of oxygenated blood to the baby during labor and delivery due to complications such as umbilical cord problems, uterine hyperstimulation, or placental issues. A hospital’s doctors and nurses can tell whether a baby is getting enough oxygen to know when to deliver in time.
An abnormal fetal heart rate is an important sign of fetal distress, which is an indication that the baby is not getting enough oxygen. If medical professionals respond to signs of fetal distress by performing a prompt emergency C-section or other interventions, they can prevent brain injuries such as hypoxic-ischemic encephalopathy (HIE) and cerebral palsy (CP).
How does fetal heart rate monitoring work?
A hospital’s doctors and nurses can observe a fetal heart rate using either an internal or external monitoring device. The internal monitor includes an electrode that is attached to the unborn baby’s scalp, while the external monitor is a belt-like device that is strapped around the mother’s abdomen.
What is normal during a contraction? When should I worry?
During a contraction, it is normal for a baby’s heart rate to drop slightly. This happens because uterine activity impinges on blood vessels and the baby gets less oxygen during the contraction. After a contraction, the heart rate should quickly return to baseline. However, if there are too many contractions, or if the contractions are too strong or last too long, the baby may be deprived of oxygen. Some signs that a baby may be experiencing a dangerous level of oxygen deprivation include:
- Tachycardia (an abnormally high heart rate)
- Bradycardia (an abnormally slow heart rate)
- Variable decelerations (sudden slowing of heart rate) that are prolonged or recurrent
- Late decelerations (a sign of placental insufficiency)
- Decreased variability
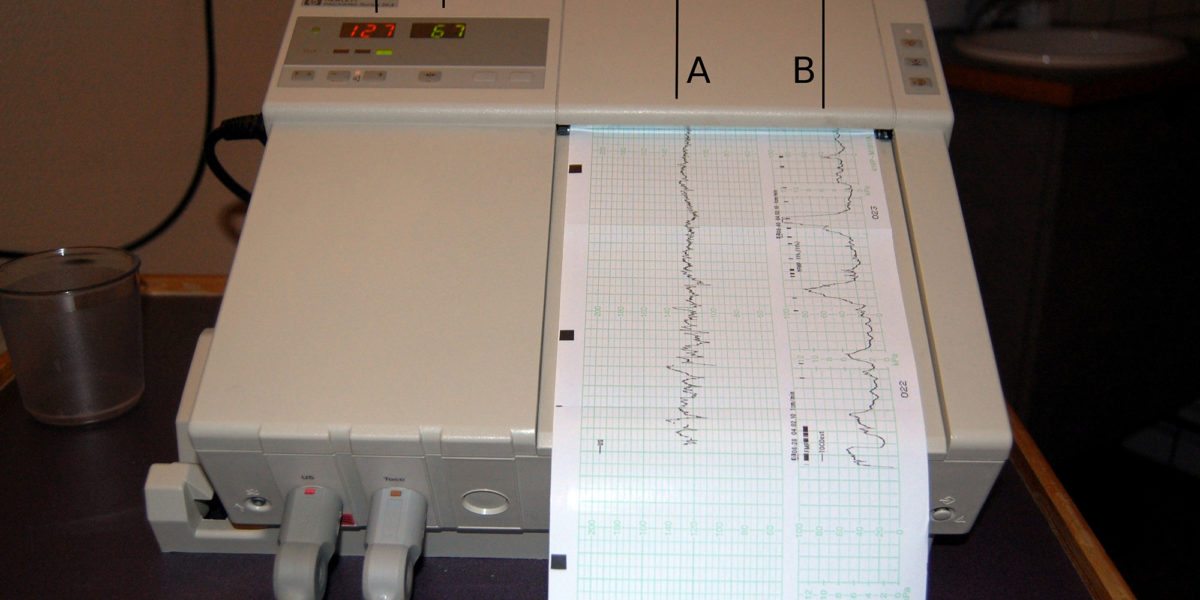
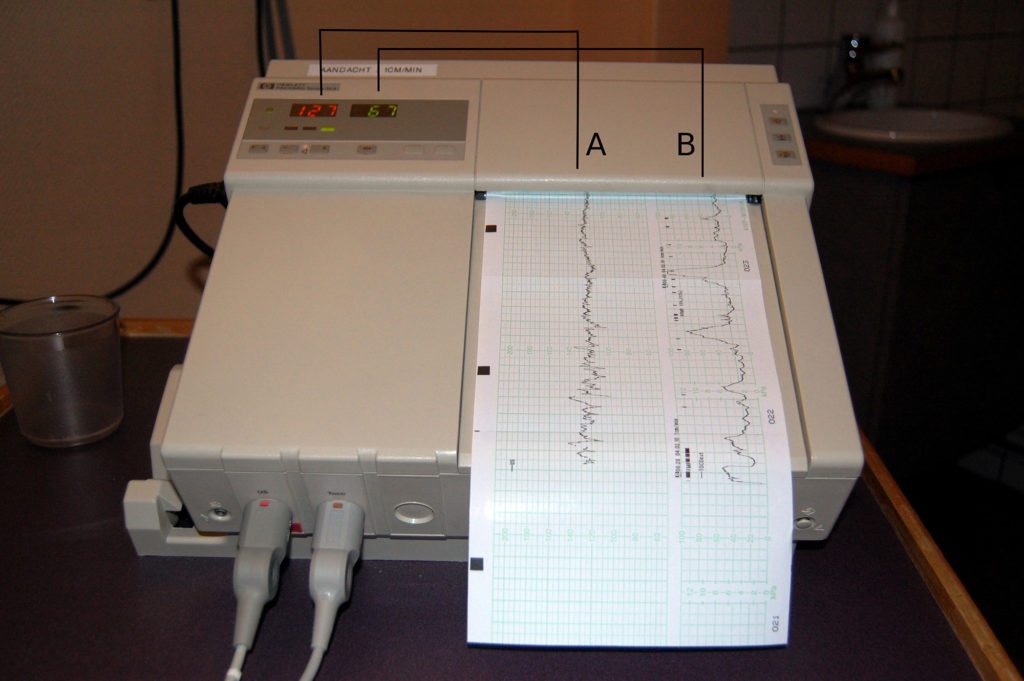
What do electronic fetal monitor (EFM) look like?
Medical staff are trained in reading the printouts (EFM tracings) that come from the electronic fetal monitoring unit. The following image is an example of EFM readings:
Citations
- Murray, DM, et al. Fetal Heart Rate Patterns in Neonatal Hypoxic-Ischemic Encephalopathy: Relationship with Early Cerebral Activity and Neurodevelopmental Outcome. Am J Perinatol. 2009 Sep;26(8):605-12. doi: 10.1055/s-0029-1220774. Epub 2009 Apr 27.
- Goulding, RM, et al. Heart Rate Variability in Hypoxic Ischemic Encephalopathy: Correlation with EEG Grade and 2-y Neurodevelopmental Outcome. Pediatric Research (2015) 77, 681–687 doi: 10.1038/pr.2015.28.