Jump To:
- APGAR Scores & HIE
- Brain Imaging
- Umbilical Cord Blood Gas Tests
- Developmental Screening
- Tests For Common Concurrent Diagnoses
- About HIE Help Center
Hypoxic-ischemic encephalopathy (HIE) can be identified at different points. In many cases, medical professionals conduct tests immediately after birth to determine if the baby has HIE. These tests occur if the medical staff suspect that HIE is possible, especially in cases of a difficult or prolonged labor, umbilical cord issues, and other events that they may suspect harbor a risk of causing oxygen deprivation-related brain damage, such as the need to resuscitate the baby after birth. This rapid diagnosis is absolutely critical for the baby because the only current treatment for hypoxic-ischemic encephalopathy, therapeutic hypothermia (also known as cooling), must be provided shortly after birth. Current guidelines say this treatment must be administered within six hours of birth/the oxygen-depriving event, and the sooner, the better. However, recent research indicates that therapeutic hypothermia may be beneficial when administered up to 24 hours after the initial brain injury; check out this post to learn more (2). Hypothermia therapy allows the baby’s brain to heal (to some degree) from hypoxic-ischemic injury, and it minimizes the severity of the baby’s disabilities. This treatment is critical to maximizing the baby’s functional abilities later in life.
In other cases, parents first become suspicious that their child may have a developmental delay when their child starts missing developmental milestones. These parents often think back to the child’s birth, wondering if something may have occurred during the process that caused the delay.
Because HIE can be identified in several different ways, there are a variety of tests doctors may use to aid in diagnosis, many of which are discussed in detail below.
APGAR scores and hypoxic-ischemic encephalopathy
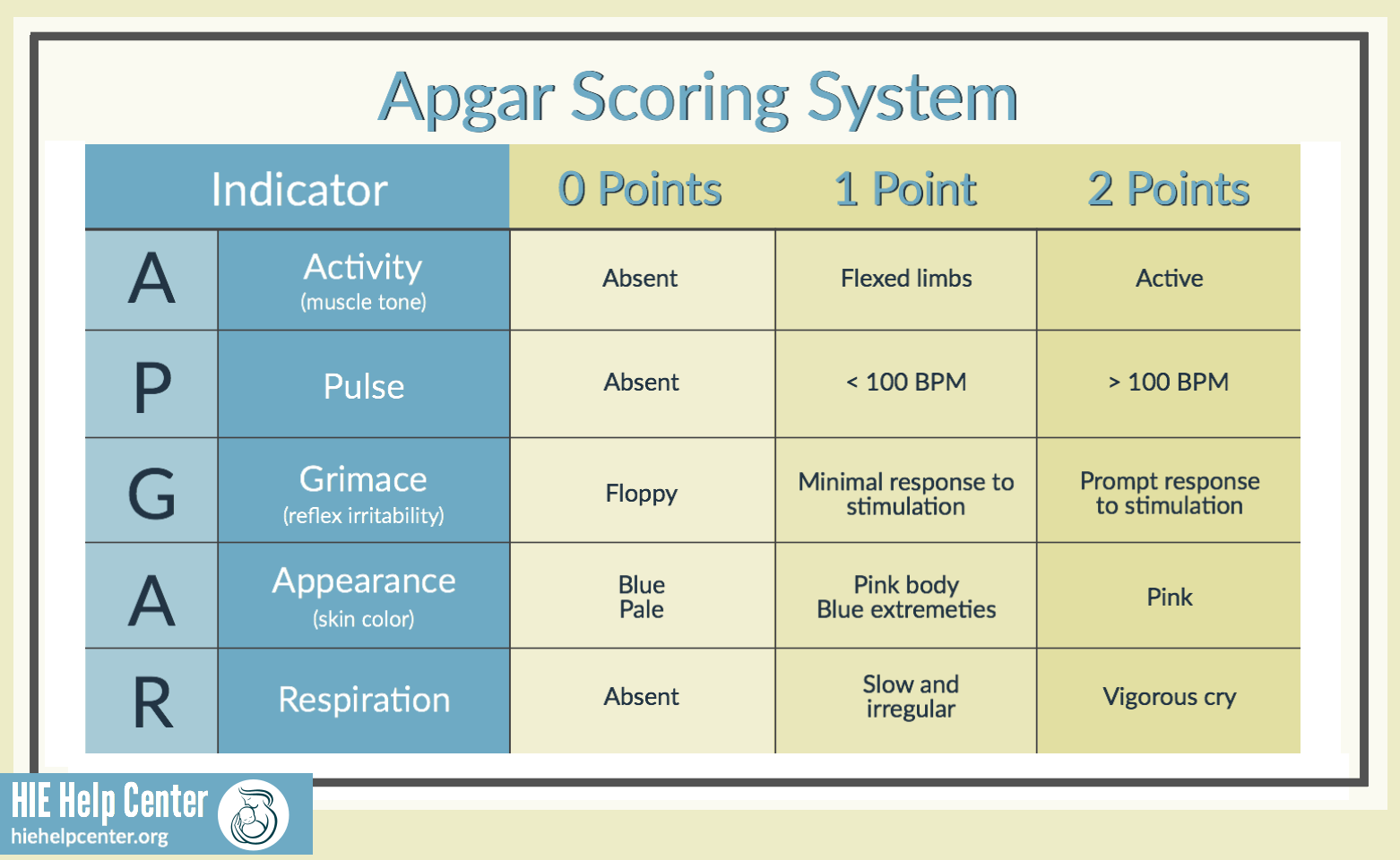
The APGAR test is a test administered to all babies when they are born. It evaluates the baby’s general health by looking at five key parameters (1):
- Appearance: This parameter looks at the baby’s skin color after birth. Physicians look to see if the baby is blue, pale, or pink all over, or if the baby is blue at the extremities.
- Pulse: This portion of the score looks at the baby’s heart rate to decide if it is slow (<100 bpm), fast (>100 bpm), or absent.
- Reflex irritability (grimace): This parameter tests the baby’s response to stimulation. Doctors decide whether the baby has no response to stimulation, responds with a feeble cry or grimace, or cries and pulls away from the stimulation.
- Activity: This evaluation tests the baby’s activity and movement. It tests whether the baby has activity and flexion (joint movement).
- Respiratory effort: This final step looks at the baby’s ability to breathe. Doctors assess whether the baby’s breathing is weak and irregular or regular and whether the baby’s cry is strong.
APGAR tests are performed at one minute after birth and five minutes after birth, and they are repeated if the score remains low afterward. Each of the five areas is evaluated on a 0-2 point scale, and the points are added up to provide a quick overall indicator of the baby’s general health (1).
The scores are broken down as follows:
- 1-3 points: Critically low
- 4-6 points: Below normal
- 7+ points: Normal APGAR score
If the baby’s APGAR scores are low and remain low, this may indicate that the baby has a brain injury like hypoxic-ischemic encephalopathy (HIE). The lower the baby’s APGAR scores, the more likely it is that the baby will need doctors to provide medical intervention (1).
Assisted APGAR scores
When APGAR scores are assigned during neonatal resuscitation, they cannot accurately be compared to scores from infants who are breathing normally, because the resuscitation will change the parameters.
In these circumstances, an “assisted” APGAR score must be used in order to factor in the resuscitation. The American College of Obstetricians and Gynecologists (ACOG) recommends using an “expanded Apgar score report form,” which can be found here (1).
How Do You Pronounce “Apgar”?
Identifying HIE through brain imaging
Brain imaging: MRIs and CT scans
MRIs and CT scans are two imaging techniques that medical professionals can use to take pictures of a baby’s brain. These scans allow trained professionals to identify if a baby has been oxygen deprived and to estimate the extent of the injury. Medical professionals can request that the baby have multiple CT scans or MRIs, to make sure they can properly track what is going on in the baby’s brain, which is a crucial step because the physical appearance of brain injuries can evolve over time (3, 4).
MRI is the best imaging method for diagnosing moderate to severe HIE. MRIs can be performed as early as 12-24 hours after birth. They accurately show injury patterns as early as 1 day after birth (sometimes sooner) and are especially useful after day 4. This method uses magnetic fields and a scanner to make a detailed image of the human brain. MRIs can identify brain lesions (regions where the brain has been damaged) and can also sometimes help doctors determine the time when a baby had a brain injury (3). MRIs do take longer than other imaging types, and there are some cases when babies can’t have an MRI (if they are unstable or are on machines that have metal in them). Some incubators and ventilators do not use metal parts, allowing some babies to have MRIs even if using a machine.
CT scans use X-rays to generate multiple ‘slices’ of images, which are ‘stacked’ together by a computer to form a 3D image of the brain’s structures. While it is not the preferred method of imaging a baby’s brain because it uses radiation and it’s not as sensitive and specific as MRI in assessing brain damage, CT scans are an alternative imaging method.
Brain imaging: Ultrasounds
Ultrasounds are another way of detecting hypoxic-ischemic encephalopathy, but this method has a lower sensitivity compared to other types of imaging. Ultrasound does not always produce an image of the outer parts of the cerebral cortex very well, and cannot always pick up on less-severe white matter abnormalities. It is, however, available at the baby’s bedside, and can show signs of hemorrhages (heavy bleeding) and abnormal ventricle sizes, as well as cerebral edema (swelling due to excess cerebrospinal fluid), increased echogenicity, and brain tissue necrosis (after 24 hours) (3, 4).
Identifying HIE through umbilical cord blood gas tests
Immediately after a baby is born (especially if the mother had a high-risk pregnancy), doctors collect an umbilical cord blood sample. Research shows that a blood sample that is taken properly can help determine whether the baby was in fetal distress (whether there was a period of time where the baby didn’t get enough oxygen).
The umbilical cord has one vein and two arteries. Blood drawn from a vein versus an artery will tell a different story; blood in the umbilical vein (which flows to the baby) reflects on oxygen flow in the uterus and placenta, while blood in the umbilical artery (which flows from the baby) reflects the fetus’ state along with the uterus and placenta (5).
The best way to test umbilical cord blood samples is from an artery (5). Medical staff clamp the cord and draw blood for testing. Once the sample is collected, there are numerous tests that can be performed. In order to determine whether the baby had a hypoxic-ischemic event, the blood’s pH is analyzed along with other factors such as PCO2, HCO3 levels, PO2, and base excess. These numbers describe the relative proportion of dissolved gases in the baby’s blood; if the arterial blood is acidotic (a condition called fetal acidosis), it means that the baby suffered an oxygen-depriving event (5).
Umbilical cord blood gas tests can also help determine what kind of acidosis occurred. This can help pinpoint what the cause of the oxygen deprivation was (5). For example, if a baby has a high PCO2 (a high level of dissolved carbon dioxide in their blood), it means that more CO2 is being produced than the baby’s body can eliminate, which can occur in cases where the umbilical cord is compressed.
Sometimes, however, if PCO2 is very different from normal values, blood gas analyzers may not accurately calculate HCO3- levels. This can cause medical staff to calculate a different value (base excess or base deficit) (5).
Umbilical cord blood gas testing isn’t always the best way to determine whether a baby likely had oxygen deprivation, however. Research has shown that some babies with HIE often have test results come back with a blood pH that is normal or very close to normal. This research also found that there can be catastrophic oxygen-depriving events that don’t show an acidic pH in the umbilical cord blood sample. If a baby has poor blood flow, it may develop acidic products in its blood, but those products won’t reach the sample site the blood was drawn from. This can also occur if the umbilical cord is occluded (blocked off completely) – if the umbilical cord is being sampled from a point downstream from an occlusion, the sample may not show any acidemia at all (6).
Almost all newborn babies with severe birth asphyxia have poor or no blood flow, which means that blood isn’t circulating well through the umbilical cord. This means that the acidic products that umbilical cord blood gas tests look for won’t be present in the sample. Functionally, this means that an umbilical cord blood gas test significantly underestimates how acidic the baby’s blood actually is (5).
Once the baby is resuscitated and their blood begins circulating better, the acidic products begin to clear their system via central circulation. Researchers found that analyzing a postnatal base deficit from a newborn within two hours of delivery is a more accurate measure of how acidic the baby’s blood was than the umbilical cord blood sample collected immediately after birth. This postnatal base deficit is a far more accurate predictor of neurological outcome than just umbilical cord blood gas testing alone (7).
Identifying HIE through developmental screening
One of the most common ways that parents obtain a diagnosis of HIE for their child is when the child begins to miss key developmental milestones. At each month and year of a baby’s life, there are certain developmental items they are generally expected to be able to do (8). If (barring genetic anomalies) a child misses a particular developmental milestone, or if a pattern of developmental delays persists, it may mean that the baby had HIE. Sometimes a baby or child may be diagnosed with cerebral palsy; the underlying cause of cerebral palsy is sometimes HIE.
The CDC has a collection of milestone checklists for new parents:
- Developmental milestones at 2 months
- Developmental milestones at 4 months
- Developmental milestones at 6 months
- Developmental milestones at 9 months
- Developmental milestones at 1 year
- Developmental milestones at 18 months
- Developmental milestones at 2 years
- Developmental milestones at 3 years
- Developmental milestones at 4 years
- Developmental milestones at 5 years
To learn more about developmental milestones and birth injury, visit the HIE Help Center’s page the topic here.
Sometimes developmental difficulties are caught early. This can happen if a baby had difficulty with feeding (latching, sucking or swallowing). It can also occur if certain developmental reflexes don’t go away when generally expected, or if they are exaggerated.
Screening generally occurs in conjunction with multiple medical and therapeutic specialists. Parents of children with HIE commonly consult pediatric neurologists, pediatricians, orthopedic surgeons, ophthalmologists, psychologists, and numerous other specialists in order to secure a diagnosis. Early diagnosis is critical for improving a child’s outcomes – the earlier a child starts therapy, the likelier it is that outcomes will be better for the child.
Tests for common concurrent diagnoses
HIE does not usually come as a single diagnosis; there can often be multiple diagnoses that a child may have. Some of the most common are intellectual and developmental delays or disabilities, as well as cerebral palsy. Sometimes children with HIE can have speech delays, motor disorders, or seizure disorders that are diagnosed first. Other times, the baby may be diagnosed with intracranial hemorrhages (brain bleeds) or fetal stroke. Occasionally, when the HIE is mild and the baby is treated with hypothermia therapy in a timely fashion, the baby may have very few to no impairments. In many cases, medical professionals run evaluations of a child once a parent has brought up developmental concerns.
Children with HIE are sometimes diagnosed with cerebral palsy. This is usually a clinical diagnosis made when a baby or child has muscle spasticity. Sometimes this is seen when a baby begins missing developmental milestones. There are two additional tests that may be helpful. Many children with cerebral palsy have seizures. EEG testing can be used to determine if a child has seizures or epilepsy, which is critical to preventing further brain damage (9). Another test that screens for coagulation problems is performed in children with hemiplegic CP or in children that show evidence of cerebral infarction (stroke) caused by HIE (10). This test determines if the child has a blood clotting disorder called prothrombotic coagulation disorder. Children with hemiparesis (weakness on one side of the body) should be tested for HIE.
About the HIE Help Center
The HIE Help Center is run by Reiter & Walsh ABC Law Centers, a medical malpractice firm exclusively handling cases involving HIE and other birth injuries. Our lawyers have over 100 years of combined experience with this type of law, and have been advocating for children with HIE and related disabilities since the firm’s inception in 1997.
We are passionate about helping families obtain the compensation necessary to cover their extensive medical bills, loss of wages (if one or both parents have to miss work in order to care for their child), assistive technology, and other necessities.
If you suspect your child’s HIE may have been caused by medical negligence, please contact us today to learn more about pursuing a case. We provide free legal consultations, during which we will inform you of your legal options and answer any questions you have. Moreover, you would pay nothing throughout the entire legal process unless we obtain a favorable settlement.
You are also welcome to reach out to us with inquiries that are not related to malpractice. We cannot provide individualized medical advice, but we’re happy to track down informational resources for you.
Citations:
- Women’s Health Care Physicians. (n.d.). Retrieved from https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/The-Apgar-Score.
- Laptook, A. R. (2017, October 24). Effects of Hypothermia in Newborns With Hypoxic-Ischemic Encephalopathy. Retrieved from https://jamanetwork.com/journals/jama/article-abstract/2658322.
- De Vries, L. S., & Groenendaal, F. (2010, June). Patterns of neonatal hypoxic-ischaemic brain injury. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2872019/.
- Heinz, E. R., & Provenzale, J. M. (2009, January). Imaging Findings in Neonatal Hypoxia: A Practical Review : American Journal of Roentgenology : Vol. 192, No. 1 (AJR). Retrieved from https://www.ajronline.org/doi/full/10.2214/AJR.08.1321.
- Simhan, H. N. (2018, January). Umbilical cord blood acid-base analysis at delivery. Retrieved from https://www.uptodate.com/contents/umbilical-cord-blood-acid-base-analysis-at-delivery.
- Yeh, & Impey. (2012, May 10). The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: Analysis of 51 519 consecutive validated samples. Retrieved from https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/j.1471-0528.2012.03335.x.
- Armstrong, L., & Stenson, B. J. (2007, November). Use of umbilical cord blood gas analysis in the assessment of the newborn. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2675384/.
- CDC’s Developmental Milestones | CDC. (n.d.). Retrieved from https://www.cdc.gov/ncbddd/actearly/milestones/.
- Epilepsy. (2019, January 23). Retrieved from https://www.mayoclinic.org/diseases-conditions/epilepsy/diagnosis-treatment/drc-20350098.
- Cerebral Palsy Workup: Approach Considerations, Potentially Helpful Laboratory Tests, Cranial Imaging Studies. (2018, October 02). Retrieved from https://emedicine.medscape.com/article/1179555-workup.