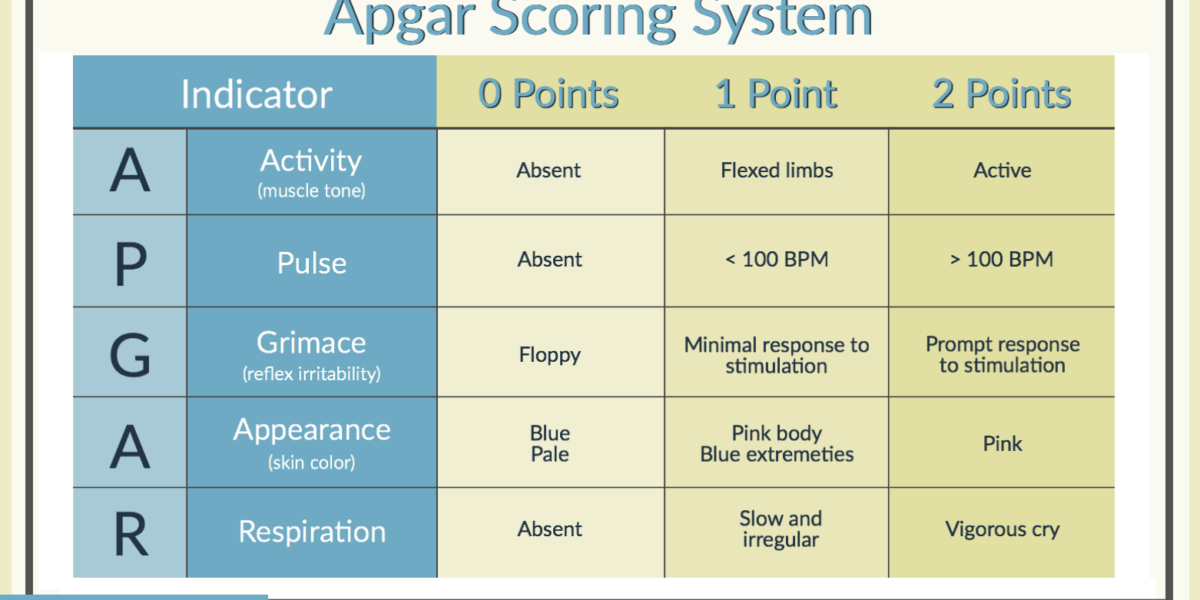
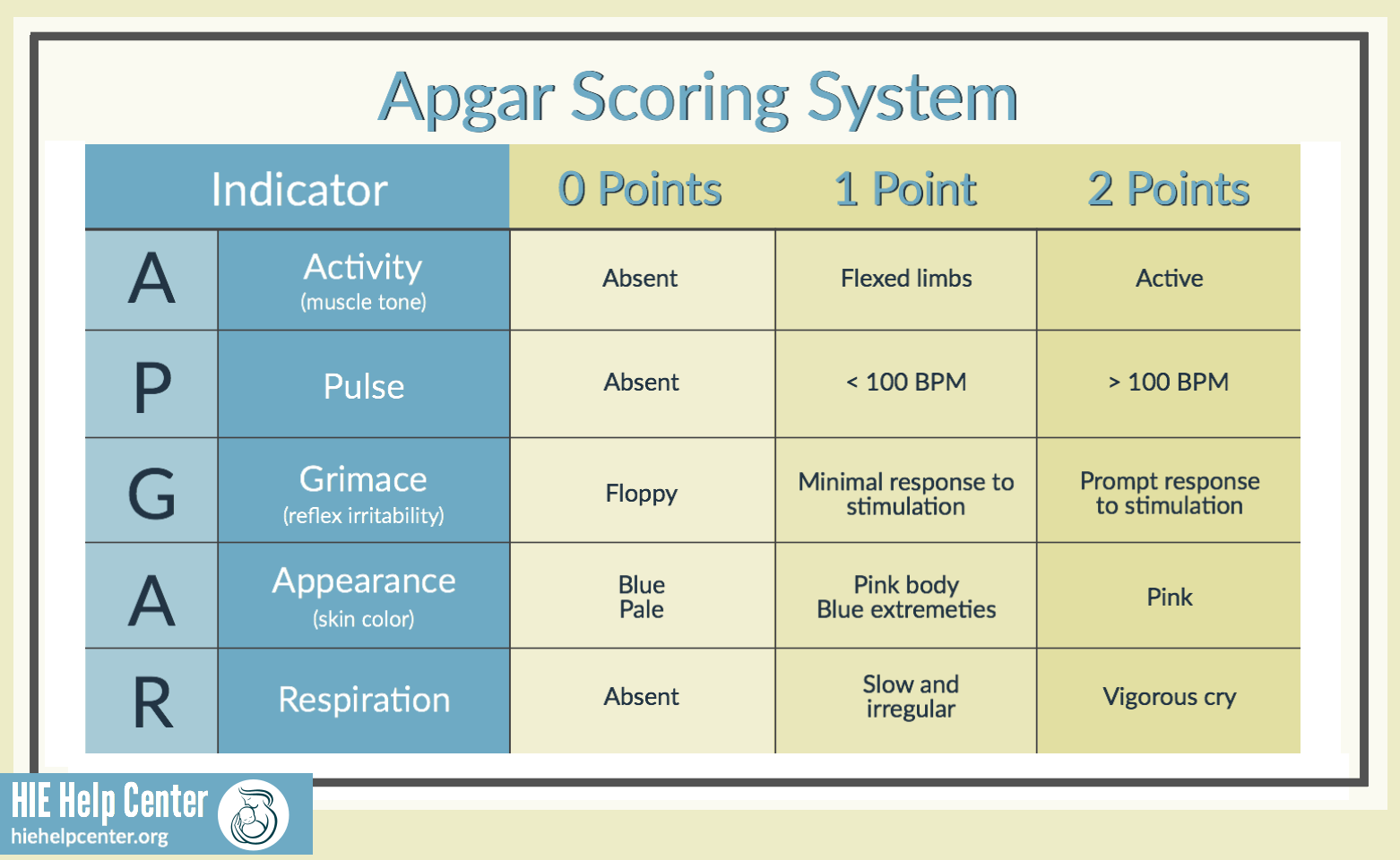
Created by Dr. Virginia Apgar in 1952, the Apgar score is a simple method of quickly assessing a newborn’s health and vital signs. The scoring system is common practice in hospitals today. There are five criteria that are assessed using the Apgar score.
 A – Appearance
A – Appearance
This is an evaluation of the baby’s skin color/tone when they are born.
- Blue, pale – 0 points
- Blue extremities, pink body – 1 point
- Pink – 2 points
P – Pulse
The medical team records the baby’s heart rate.
- Absent heart rate – 0 points
- Slow heart rate (below 100 bpm) – 1 point
- Fast heart rate (over 100 bpm) – 2 points
 G – Grimace
G – Grimace
The medical team notes how the baby responds to stimuli.
- Floppy/no response – 0 points
- Minimal response to stimuli – 1 point
- Prompt response to stimuli – 2 points
A – Activity
The medical team notes the baby’s muscle tone/activity level.
- Absent – 0 points
- Flexed arms and legs – 1 point
- Active – 2 points
 R – Respiration
R – Respiration
The medical team notes the baby’s breathing ability.
- Not breathing – 0 points
- Slow and irregular breathing – 1 point
- Vigorous cry – 2 points
How is an Apgar score calculated?
The five criteria are each scored as 0, 1, or 2 (two being the best), and the total score is calculated by then adding the five values obtained. Apgar scores are taken at the 1, 5, and 10 minute intervals.
What do Apgar scores mean?
- Scores of 0-3 are considered critical, especially in babies born at or near term
- Scores of 4-6 are considered below normal and indicate that the medical intervention is likely required
- Scores of 7+ are considered normal
There is evidence to suggest that infants whose Apgar scores remain low at five minutes or later are much more likely to suffer long-term neurological damage.
What is a good Apgar score?
A high Apgar score (closer to 10) is generally considered better than a low Apgar score (closer to 0). Babies with lower Apgar scores are more likely than babies with higher scores to need resuscitation. Sometimes, however, resuscitation must occur before an Apgar score is taken.
Assisted Apgar scores
If an infant undergoes resuscitation, the Apgar score given during resuscitation will not be the same as that given to a baby breathing on their own. Therefore, many have suggested that an assisted Apgar score be given to resuscitated babies. This score would account for resuscitation.
What’s the relationship between Apgar scores, asphyxia, and HIE?
Asphyxia is the marked impairment of gas exchange, which can, if prolonged, lead to progressive hypoxemia and other complications. An Apgar score alone cannot diagnose asphyxia. A low Apgar score can simply mean that a baby is immature, not necessarily that they are suffering from asphyxia. However, continued lower Apgar scores can be evidence of asphyxia and hypoxic-ischemic encephalopathy (HIE). The lower the Apgar score, the more alert the medical team should be to the possibility of the baby requiring intervention.
Higher Apgar scores, however, do not rule out the possibility that the baby has a brain injury, such as HIE. In all cases, physicians must recognize other signs and symptoms of damage in order to treat them both quickly and appropriately.
Other signs and symptoms of HIE
- Fetal heart rate patterns and abnormalities
- Clinical cerebral function
- Placental pathology
- Multisystem organ function
- Neuroimaging studies
- Neonatal electroencephalography
About Our Team
The HIE Help Center is an informational resource created by nurses and attorneys at ABC Law Centers. For over 25 years, our team has solely taken on legal cases that involve birth injuries, specifically those involving hypoxic-ischemic encephalopathy. Was your child diagnosed with HIE or a related birth injury? We can help! Give us a call today.
Sources:
- Women’s Health Care Physicians. (n.d.). Retrieved from https://www.acog.org/Clinical-Guidance-and-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/The-Apgar-Score
- (n.d.). Retrieved from https://www.uptodate.com/contents/overview-of-the-routine-management-of-the-healthy-newborn-infant#H3