During pregnancy, the umbilical cord supplies the baby with oxygen and nutrients. If the cord is unable to do its job because it is being compressed or otherwise damaged, the consequences can be life-threatening. A disruption in the flow of oxygenated blood to the baby can result in birth injuries such as hypoxic-ischemic encephalopathy and cerebral palsy. There are several cord-related pregnancy complications that restrict oxygen supply to the baby, such as:
- Nuchal cord
- Umbilical cord prolapse
- Short cord
- True knot
- Infected or inflamed cord
- Vasa previa
Nuchal cord and HIE
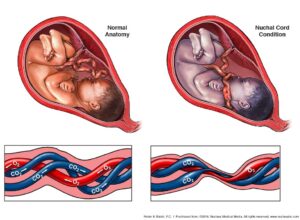
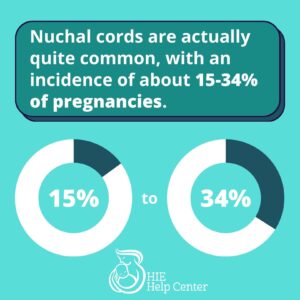 A nuchal cord occurs when the umbilical cord is wrapped one or more times around the baby’s neck. This condition is actually quite common, with an incidence of about 15-34% of pregnancies (1). Sometimes the issue resolves itself; other times it persists throughout labor and delivery.
A nuchal cord occurs when the umbilical cord is wrapped one or more times around the baby’s neck. This condition is actually quite common, with an incidence of about 15-34% of pregnancies (1). Sometimes the issue resolves itself; other times it persists throughout labor and delivery.
Tightly wrapped nuchal cords are dangerous because they can strangle the baby. Also, if the cord becomes compressed against itself or the baby’s neck, this can cut off their oxygen supply.
Common risk factors for nuchal cord formation include (1, 2):
- Long umbilical cord length
- An especially active fetus
- Excessive amniotic fluid (polyhydramnios)
- Multiples sharing an amniotic sac (cords of twins or other multiples may become tangled around their own necks or their siblings’ necks)
Learn more about the connections about nuchal cord and HIE.
Signs and diagnosis of nuchal cords
If a baby’s movement slows after 37 weeks gestation, that is a warning sign that there may be a nuchal cord (2). Another indication is a decreased fetal heart rate.
Nuchal cords are often diagnosed by looking at ultrasound images. It may be necessary for doctors to look at the fetal neck from multiple angles. If an umbilical cord is seen around at least ¾ of the neck, that constitutes a nuchal cord (1). It is important to note that ultrasounds are not 100% accurate at detecting nuchal cords.
Treatment/management of nuchal cords
Sometimes, nuchal cords can be managed by a medical professional reaching into the birth canal and maneuvering the cord so that it is no longer wrapped around the baby’s neck (1). If the cord is wrapped too tightly to do this, it may be clamped and cut after the baby’s head is delivered. In certain cases, an emergency C-section may be necessary.
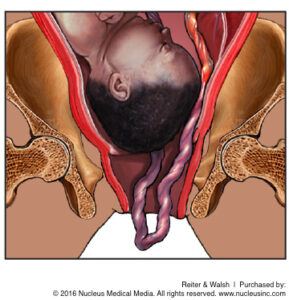
Cord prolapse and HIE
In a healthy vaginal birth, the baby exits the cervix first, and the umbilical cord follows the baby down the birth canal. Umbilical cord prolapse is a condition in which the cord emerges before or alongside the baby (3). This is dangerous because the cord can easily become compressed between the baby’s body and the birth canal, restricting or cutting off oxygen supply to the baby.
Common risk factors for cord prolapse can include (3):
 Premature rupture of membranes: If the mother’s water breaks too early, when the baby is still positioned high in the uterus, the umbilical cord may make its way into the birth canal before the baby can descend.
Premature rupture of membranes: If the mother’s water breaks too early, when the baby is still positioned high in the uterus, the umbilical cord may make its way into the birth canal before the baby can descend.- Long umbilical cord length
- Low birth weight
- Pelvic deformities
- Low lying placenta
- Malpresentation (e.g. breech)
- Multiples sharing an amniotic sac: The first baby to be born may drag the cord of another through the birth canal.
- Premature delivery
- Prolonged labor
- Uterine malformations
- External fetal anomalies
- Unengaged presenting part
- Excessive amniotic fluid (polyhydramnios): This may push the cord down before the baby.
Signs and diagnosis
The clearest sign of a cord prolapse is the emergence of the cord prior to the baby. However, this does not always happen, as the cord can also come down the canal alongside the baby. Signs of fetal distress, such as heart rate deceleration, also clue medical professionals into the possibility of cord prolapse.
Treatment/management of cord prolapse
Sometimes, it is possible for a physician to move the baby away from the cord, possibly with the help of forceps or a vacuum extractor (which can also be dangerous for the baby). However, this often fails, and then an emergency C-section delivery is necessary. While preparing the mother for surgery, medical professionals will often opt to push the presenting part of the baby back into the pelvis.
Short cord and HIE
The average umbilical cord length is between 55 and 60 cm. An umbilical cord is considered short if it is 35 cm or less in length (4). Short umbilical cords occur in roughly 6% of pregnancies. They are risky because they can affect the growth and development of the baby as well as the outcome of the pregnancy. Short umbilical cords can lead to many complications, including (4):
 Prolonged labor
Prolonged labor- Placental abruption
- Hypoxic-ischemic encephalopathy (HIE)
- Cerebral palsy
- Intrauterine growth restriction (IUGR)
- Umbilical cord rupture
Risk factors for short cord
Some of the risk factors for short umbilical cord include (4):
- Gestational diabetes
- Maternal low body mass index (BMI)
- Oligohydramnios (decreased amniotic fluid)
- Polyhydramnios (excessing amniotic fluid)
- History of smoking during pregnancy
Signs and diagnosis of short cord
Short cord should be suspected if there is low fetal movement; this could both cause and be caused by short cord. Signs of fetal distress should also prompt medical professionals to check for short cord (as well as a number of other birth complications). The length of the umbilical cord can be determined through ultrasound examination. If the cord is short, the mother should be monitored closely for the rest of her pregnancy.
Treatment/management of short cord
If the cord is extremely short, or there are signs of fetal distress, the mother may be admitted to the hospital for inpatient monitoring prior to delivery. If she is diagnosed with placental abruption or the baby is in fetal distress, then the medical team should quickly prepare the mother for emergency C-section.
True knot and HIE
The name of this condition, “true knot,” is somewhat self explanatory: it is a knot that forms in the umbilical cord. This can happen when babies move around in the womb. True knot affects about 0.3-2% of pregnancies (5). A true knot becomes especially dangerous when fetal movement stretches the umbilical cord and tightens the knot. This causes vessels in the umbilical cord to become compressed, and limits oxygen supply to the baby.
 Common risk factors for true knot can include (5):
Common risk factors for true knot can include (5):
- Twins sharing an amniotic sac
- Excessive amniotic fluid (polyhydramnios)
- A mother who has previously been pregnant two or more times
- A mother who is older than 35
- Long umbilical cord
- Small size fetus
Signs and diagnosis of true knot
Fetuses connected to an umbilical cord with a true knot may show decreased movement after week 37 of pregnancy. There may also be signs of fetal distress, such as an abnormal heart rate. Usually, diagnosis of a true knot happens through an ultrasound examination. If risk factors for a true knot are present, more frequent ultrasounds are typically indicated.
Treatment/management of true knot
If medical professionals diagnose a true knot, they should closely monitor fetal health. Often, the mother will be admitted to the hospital for observation, and so that emergency intervention can be performed if the knot tightens and the fetus begins to exhibit signs of distress. Usually, this would involve an emergency C-section.
Funisitis and HIE
Sometimes, maternal infections can develop in the placenta and spread to the umbilical cord, causing cord inflammation. Umbilical cord infection and inflammation is known as funisitis (6). Though inflammation of the chorioamniotic membranes, a condition called chorioamnionitis, is a maternal response to bacteria, funisitis is a fetal response. Sometimes, this is not a severe issue. However, much like other cord problems, funisitis can limit oxygen flow, resulting in serious complications. Chorioamnionitis and funisitis can also increase the chances of preterm labor and neonatal sepsis.
Common risk factors for funisitis
- Prolonged labor: The more time spent in labor at a cervical dilation of more than 4 cm, the higher the chances of chorioamnionitis (6)
- Chorioamnionitis is also more common in mothers who experience (7):
- Cervical insufficiency
- Meconium-stained amniotic fluid
- Alcohol and tobacco use
- Previous chorioamnionitis
- Presence of pathogens in the genital tract (Group B Strep, bacterial vaginosis, etc.)
- Internal fetal monitoring
- Nulliparity
- Several vaginal exams
Signs and diagnosis of funisitis
Funisitis can be diagnosed through cord examination and tests of fetal and maternal blood. Peripheral funisitis looks like small, white or yellow plaques on the outside of the umbilical cord; necrotizing funisitis looks like rings on the cut surface of the cord (8).
Treatment/management of funisitis
Funisitis can cause the flow of oxygen and nutrients to the baby to become compromised, especially if delivery doesn’t happen in a timely fashion. Birth asphyxia can result. If funisitis is very severe, delivery via emergency C-section may be necessary. The infant will also likely need antibiotic treatment.
Vasa previa and HIE
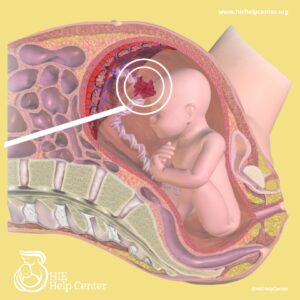
In a healthy pregnancy, fetal blood vessels run through the umbilical cord, connecting the infant to the placenta. Vasa previa is a condition in which fetal vessels move out of the umbilical cord’s protection and travel through the membranes that lie across the birth canal. This can happen for one of these two reasons:
- The cord implants in the fetal membranes instead of the placenta, and the fetal vessels need to get to the placenta.
- The placenta is divided into two “lobes” and the vessels must connect the two.
Vasa previa is a dangerous condition because the unprotected fetal vessels may end up rupturing along with the amniotic sac. If this happens, it can lead to massive fetal blood loss.
Risk factors for vasa previa can include (9):
- Accessory placental lobes
- Multiples
- Low-lying placenta or placenta previa (at any point during pregnancy)
- In Vitro Fertilization (IVF) pregnancies
- Velamentous insertion of the cord
Signs and diagnosis of vasa previa
 Vasa previa can be diagnosed through a transvaginal ultrasound with color Doppler (9). If it is not diagnosed early, it should be suspected if the mother bleeds when her water breaks, or if the baby’s heart rate is abnormal.
Vasa previa can be diagnosed through a transvaginal ultrasound with color Doppler (9). If it is not diagnosed early, it should be suspected if the mother bleeds when her water breaks, or if the baby’s heart rate is abnormal.
Treatment/management of vasa previa
Once a mother has a vasa previa diagnosis, she should be carefully monitored. Because vasa previa increases the risk of preterm delivery, she should also be given a steroid called betamethasone, which will help the baby’s tissues mature. Between 30-32 weeks of gestation, she should be admitted to the hospital for more frequent testing. Usually, C-section is scheduled for about 35 weeks gestation.
Should I contact an attorney?
If medical professionals fail to diagnose an umbilical cord problem in a timely fashion, do not respond with appropriate intervention (such as an emergency C-section), or do not provide hypothermia therapy, the child may be entitled to compensation from a medical malpractice lawsuit. Compensation from successful medical malpractice cases helps to defray to costs of specialized care and resources.
Disclaimer: The information presented above is intended only to be a general educational resource. It is not intended to be (and should not be interpreted as) medical advice. If you have questions about an umbilical cord problem, please consult with a medical professional.
About the HIE Help Center
The HIE Help Center is run by ABC Law Centers, a medical malpractice firm exclusively handling cases involving HIE and other birth injuries. Our lawyers have over 100 years of combined experience with this type of law, and have been advocating for children with HIE and related disabilities since the firm’s inception in 1997.
If you suspect your child’s HIE may have been caused by medical negligence, please contact us today to learn more about pursuing a case. We provide free legal consultations, during which we will inform you of your legal options and answer any questions you have. Moreover, you would pay nothing throughout the entire legal process unless we obtain a favorable settlement.
You are also welcome to reach out to us with inquiries that are not related to malpractice. We cannot provide individualized medical advice, but we’re happy to track down informational resources for you.
Sources
- Schaffer, L., & Zimmermann, R. (2023, November 15). Nuchal cord. Retrieved May 13, 2024, from https://www.uptodate.com/contents/nuchal-cord
- What to Expect, E. (2022, October 17). Cord Knots During Pregnancy. Retrieved May 13, 2024, from https://www.whattoexpect.com/pregnancy/pregnancy-health/complications/cord-knots.aspx
- Bush, M., Eddleman, K., & Belogolovkin, V. (n.d.). Retrieved May 8, 2024, from https://www.uptodate.com/contents/umbilical-cord-prolapse
- Short Umbilical Cord. (2018, December 14). Retrieved May 9, 2024, from https://www.dovemed.com/diseases-conditions/short-umbilical-cord/
- Ikechebelu, J., Eleje, G., & Ofojebe, C. (2014). True umbilical cord knot leading to fetal demise. Annals of medical and health sciences research, 4(Suppl 2), S155–S158. doi:10.4103/2141-9248.138044
- Kim, C. J., Romero, R., Chaemsaithong, P., Chaiyasit, N., Yoon, B. H., & Kim, Y. M. (2015, October). Acute chorioamnionitis and funisitis: Definition, pathologic features, and clinical significance. Retrieved May 7, 2024, from https://www.ncbi.nlm.nih.gov/pubmed/26428501
- Tita, A. T. (2024, April 8). Clinical chorioamnionitis. Retrieved from https://www.uptodate.com/contents/clinical-chorioamnionitis
- Kowalski, P. J. (2021, December 16). Umbilical vasculitis and funisitis. Retrieved May 13, 2024, from https://www.pathologyoutlines.com/topic/placentaacutefunisitis.html
- Datta, S., Babu, K. M., Mitra, S., & Patil, D. (2016). Vasa Previa: An Avoidable Obstetric Tragedy. Journal of obstetrics and gynaecology of India, 66(3), 185–187. doi:10.1007/s13224-015-0751-4

